Exploring the legal landscape of collaborating physicians for nurse practitioners across different states unveils a complex web of regulations and obligations. Dive into this comprehensive guide to understand the nuances and implications of state-specific requirements.
Legal Requirements for Collaborating Physicians
The role of collaborating physicians for nurse practitioners is crucial in providing quality healthcare services. Collaborating physicians work together with nurse practitioners to oversee patient care, provide guidance, and ensure compliance with state regulations.Legal Obligations of Collaborating Physicians
Collaborating physicians have legal obligations in different states, which may include but are not limited to:- Signing collaborative agreements with nurse practitioners
- Reviewing and approving patient care plans
- Ensuring proper supervision and consultation with nurse practitioners
- Complying with state-specific regulations and scope of practice laws
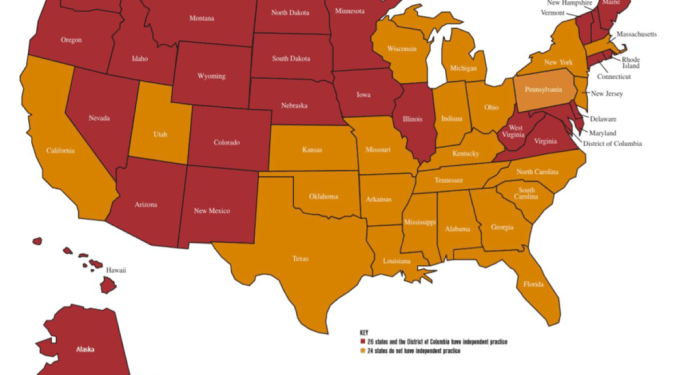
Specific State Requirements for Collaborating Physicians
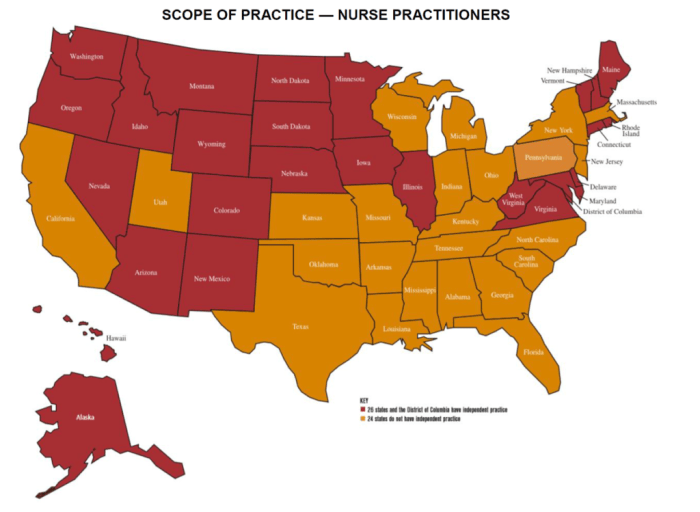
Each state has specific requirements set by laws for collaborating physicians, which can vary widely. Some states may require collaborating physicians to be physically present during patient consultations, while others may allow for supervision through telecommunication. It is essential for collaborating physicians to be aware of and comply with the specific requirements in the state where they practice.State-specific Regulations
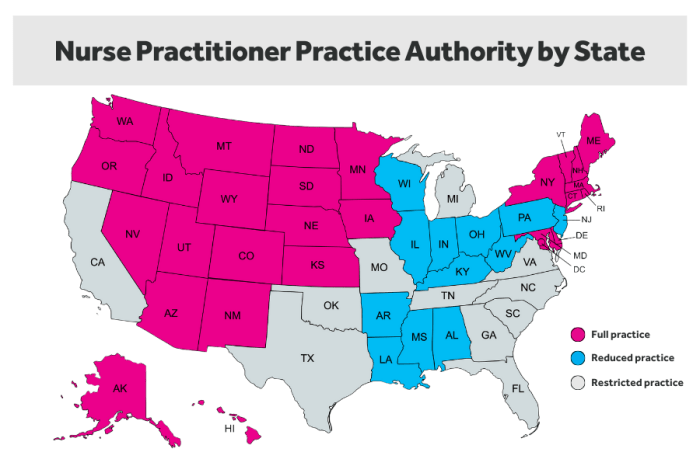
When it comes to collaborating physician requirements, each state may have its own set of regulations that nurse practitioners and collaborating physicians must adhere to. These regulations can vary significantly from state to state, impacting the way healthcare is delivered and the scope of practice for nurse practitioners.
Comparison of State Regulations
- In some states, collaborating physicians are required to be physically present for a certain percentage of the time when working with nurse practitioners, while in others, virtual collaboration may be allowed.
- States may differ in the number of nurse practitioners a collaborating physician can oversee at a given time.
- The level of oversight and supervision required by collaborating physicians can also vary, with some states allowing more autonomy for nurse practitioners.
Examples of Varying State Laws
- In California, collaborating physicians must be available by phone or electronic communication at all times, while in Texas, face-to-face meetings are required at least once a month.
- Some states may have specific training or certification requirements for collaborating physicians, while others may not have such mandates.
Implications of Differing State Regulations
- The varying state regulations can impact the ability of nurse practitioners to practice to the full extent of their education and training.
- Certain state regulations may create barriers for nurse practitioners to provide care in rural or underserved areas where collaborating physicians may be limited.
- Collaborating physicians may need to be aware of and comply with different regulations if they work across multiple states, adding complexity to their practice.
Collaborative Agreement Details
Collaborative agreements between nurse practitioners and collaborating physicians are essential components of the healthcare team. These agreements Artikel the terms of the collaboration and the responsibilities of each party involved.
Key Components of a Collaborative Agreement
- Scope of practice for the nurse practitioner
- Supervision requirements for the collaborating physician
- Protocols for communication and consultation
- Process for patient referrals
- Quality assurance measures
Importance of Collaborative Agreements
Collaborative agreements provide a framework for the nurse practitioner to practice to the full extent of their education and training while ensuring patient safety and quality care
Ensuring Compliance with State Regulations
Collaborative agreements are crucial for ensuring compliance with state regulations regarding nurse practitioner practice. By clearly outlining the roles and responsibilities of each party, these agreements help meet the specific requirements set forth by each state's regulatory bodies, maintaining legal and ethical standards in healthcare delivery.
Supervision and Oversight
 In the collaborative relationship between nurse practitioners and collaborating physicians, the level of supervision and oversight plays a crucial role in ensuring quality patient care and adherence to legal requirements.
In the collaborative relationship between nurse practitioners and collaborating physicians, the level of supervision and oversight plays a crucial role in ensuring quality patient care and adherence to legal requirements.Role of Collaborating Physicians in Supervision
- Collaborating physicians are required to provide oversight and supervision to nurse practitioners as per state regulations.
- They review patient cases, provide guidance on complex medical issues, and ensure that care provided by nurse practitioners meets the standard of care.
- Physicians may need to be available for consultation or in-person supervision depending on state laws.
Support Mechanisms for Nurse Practitioners
- Collaborating physicians support nurse practitioners by offering clinical advice, sharing knowledge and expertise, and assisting in decision-making processes.
- They may conduct periodic chart reviews, provide feedback on practice patterns, and help nurse practitioners develop their clinical skills.
- Physicians also play a role in ensuring that nurse practitioners comply with state regulations and maintain a high standard of care.
Impact on Collaboration
- The supervision requirements can impact the autonomy of nurse practitioners and the flexibility of their practice.
- Clear communication, mutual respect, and a collaborative approach are essential for a successful working relationship between nurse practitioners and collaborating physicians.
- Effective supervision can enhance patient outcomes, improve care coordination, and promote a culture of continuous learning and professional development.
Ultimate Conclusion
As we conclude this discussion on collaborating physicians for nurse practitioners, it's clear that navigating the legal requirements by state is crucial for ensuring seamless collaboration and quality patient care. Stay informed and compliant to foster a successful partnership between nurse practitioners and collaborating physicians.
FAQ Section
What are the key legal obligations of collaborating physicians for nurse practitioners?
Collaborating physicians are required to provide oversight, support, and guidance to nurse practitioners to ensure quality patient care and compliance with state laws.
How do state laws vary in terms of collaborating physician regulations?
State laws differ in the level of supervision required, the specifics of collaborative agreements, and the extent of oversight collaborating physicians must provide.
Why are collaborative agreements important for nurse practitioners?
Collaborative agreements Artikel the working relationship between nurse practitioners and collaborating physicians, ensuring adherence to state regulations and promoting effective teamwork.